Weight Loss
Information on Weight Loss
Weight Loss
Weight loss, in the context of medicine, health, or physical fitness, refers to a reduction of the total body mass, due to a mean loss of fluid, body fat or adipose tissue or lean mass, namely bone mineral deposits, muscle, tendon, and other connective tissue. Weight loss can either occur unintentionally due to malnourishment or an underlying disease or arise from a conscious effort to improve an actual or perceived overweight or obese state. "Unexplained" weight loss that is not caused by reduction in calorific intake or exercise is called cachexia and may be a symptom of a serious medical condition. Intentional weight loss is commonly referred to as slimming.
Techniques
The least intrusive weight loss methods, and those most often recommended, are adjustments to eating patterns and increased physical activity, generally in the form of exercise. The World Health Organization recommended that people combine a reduction of processed foods high in saturated fats, sugar and salt and caloric content of the diet with an increase in physical activity.
An increase in fiber intake is also recommended for regulating bowel movements. Other methods of weight loss include use of drugs and supplements that decrease appetite, block fat absorption, or reduce stomach volume. Bariatric surgery may be indicated in cases of severe obesity. Two common bariatric surgical procedures are gastric bypass and gastric banding. Both can be effective at limiting the intake of food energy by reducing the size of the stomach, but as with any surgical procedure both come with their own risks that should be considered in consultation with a physician. Dietary supplements, though widely used, are not considered a healthy option for weight loss. Many are available, but very few are effective in the long term.
Virtual gastric band uses hypnosis to make the brain think the stomach is smaller than it really is and hence lower the amount of food ingested. This brings as a consequence weight reduction. This method is complemented with psychological treatment for anxiety management and with hypnopedia. Research has been conducted into the use of hypnosis as a weight management alternative. In 1996 a study found that cognitive-behavioral therapy (CBT) was more effective for weight reduction if reinforced with hypnosis. Acceptance and Commitment Therapy ACT, a mindfulness approach to weight loss, has also in the last few years been demonstrating its usefulness.
Weight loss issues related to specific diseases
· As chronic obstructive pulmonary disease (COPD) advances, about 35% of patients experience severe weight loss called pulmonary cachexia, including diminished muscle mass. Around 25% experience moderate to severe weight loss, and most others have some weight loss. Greater weight loss is associated with poorer prognosis. Theories about contributing factors include appetite loss related to reduced activity, additional energy required for breathing, and the difficulty of eating with dyspnea (labored breathing).
· Cancer, a very common and sometimes fatal cause of unexplained (idiopathic) weight loss. About one-third of unintentional weight loss cases are secondary to malignancy. Cancers to suspect in patients with unexplained weight loss include gastrointestinal, prostate, hepatobiliary (hepatocellular carcinoma, pancreatic cancer), ovarian, hematologic or lung malignancies.
· People with HIV often experience weight loss, and it is associated with poorer outcomes. Wasting syndrome is an AIDS-defining condition.
· Gastrointestinal disorders are another common cause of unexplained weight loss – in fact they are the most common non-cancerous cause of idiopathic weight loss.[citation needed] Possible gastrointestinal etiologies of unexplained weight loss include: celiac disease, peptic ulcer disease, inflammatory bowel disease (crohn's disease and ulcerative colitis), pancreatitis, gastritis, diarrhea and many other GI conditions.
· Infection. Some infectious diseases can cause weight loss. Fungal illnesses, endocarditis, many parasitic diseases, AIDS, and some other subacute or occult infections may cause weight loss.
· Renal disease. Patients who have uremia often have poor or absent appetite, vomiting and nausea. This can cause weight loss.
· Cardiac disease. Cardiovascular disease, especially congestive heart failure, may cause unexplained weight loss.
· Connective tissue disease.
· Neurologic disease, including dementia.
· Oral, taste or dental problems (including infections) can reduce nutrient intake leading to weight loss.
Therapy
Medical treatment can directly or indirectly cause weight loss, impairing treatment effectiveness and recovery that can lead to further weight loss in a vicious cycle. Many patients will be in pain and have a loss of appetite after surgery. Part of the body's response to surgery is to direct energy to wound healing, which increases the body's overall energy requirements. Surgery affects nutritional status indirectly, particularly during the recovery period, as it can interfere with wound healing and other aspects of recovery. Surgery directly affects nutritional status if a procedure permanently alters the digestive system. Enteral nutrition (tube feeding) is often needed. However, a policy of 'nil by mouth' for all gastrointestinal surgery has not been shown to benefit, with some suggestion it might hinder recovery. Early post-operative nutrition is a part of Enhanced Recovery After Surgery protocols. These protocols also include carbohydrate loading in the 24 hours before surgery, but earlier nutritional interventions have not been shown to have a significant impact.
Some medications can cause weight loss, while others can cause weight gain

Polycystic Ovary Syndrome
Information on Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a condition that affects a woman’s hormone levels.
Women with PCOS produce higher-than-normal amounts of male hormones. This hormone imbalance causes them to skip menstrual periods and makes it harder for them to get pregnant.
PCOS also causes hair growth on the face and body, and baldness. And it can contribute to long-term health problems like diabetes and heart disease.
Birth control pills and diabetes drugs can help fix the hormone imbalance and improve symptoms.
Read on for a look at the causes of PCOS and its effects on a woman’s body.
What is PCOS?
PCOS is a problem with hormones that affects women during their childbearing years (ages 15 to 44). Between 2.2 and 26.7 % of women in this age group have PCOS.
Many women have PCOS but don’t know it. In one study, up to 70 % of women with PCOS hadn’t been diagnosed (2).
PCOS affects a woman’s ovaries, the reproductive organs that produce estrogen and progesterone — hormones that regulate the menstrual cycle. The ovaries also produce a small number of male hormones called androgens.
The ovaries release eggs to be fertilized by a man’s sperm. The release of an egg each month is called ovulation.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) control ovulation. FSH stimulates the ovary to produce a follicle — a sac that contains an egg — and then LH triggers the ovary to release a mature egg.
PCOS is a “syndrome,” or group of symptoms that affects the ovaries and ovulation. Its three main features are:
• cysts in the ovaries
• high levels of male hormones
• irregular or skipped periods
In PCOS, many small, fluid-filled sacs grow inside the ovaries. The word “polycystic” means “many cysts.”
These sacs are actually follicles, each one containing an immature egg. The eggs never mature enough to trigger ovulation.
The lack of ovulation alters levels of estrogen, progesterone, FSH, and LH. Estrogen and progesterone levels are lower than usual, while androgen levels are higher than usual.
Extra male hormones disrupt the menstrual cycle, so women with PCOS get fewer periods than usual.
PCOS isn’t a new condition. Italian physician Antonio Vallisneri first described its symptoms in 1721.
What causes it?
Doctors don’t know exactly what causes PCOS. They believe that high levels of male hormones prevent the ovaries from producing hormones and making eggs normally.
Genes, insulin resistance, and inflammation have all been linked to excess androgen production.
· Genes
Studies show that PCOS runs in families.
It’s likely that many genes — not just one — contribute to the condition.
Insulin resistance
Up to 70 % of women with PCOS have insulin resistance, meaning that their cells can’t use insulin properly.
Insulin is a hormone the pancreas produces to help the body use sugar from foods for energy.
When cells can’t use insulin properly, the body’s demand for insulin increases. The pancreas makes more insulin to compensate. Extra insulin triggers the ovaries to produce more male hormones.
Obesity is a major cause of insulin resistance. Both obesity and insulin resistance can increase your risk for type 2 diabetes.
· Inflammation
Women with PCOS often have increased levels of inflammation in their body. Being overweight can also contribute to inflammation. Studies have linked excess inflammation to higher androgen levels.
Common symptoms of PCOS
Some women start seeing symptoms around the time of their first period. Others only discover they have PCOS after they’ve gained a lot of weight or they’ve had trouble getting pregnant.
The most common PCOS symptoms are:
• Irregular periods. A lack of ovulation prevents the uterine lining from shedding every month. Some women with PCOS get fewer than eight periods a year.
• Heavy bleeding. The uterine lining builds up for a longer period of time, so the periods you do get can be heavier than normal.
• Hair growth. More than 70 % of women with this condition grow hair on their face and body — including on their back, belly, and chest (11). Excess hair growth is called hirsutism.
• Acne. Male hormones can make the skin oilier than usual and cause breakouts on areas like the face, chest, and upper back.
• Weight gain. Up to 80 % of women with PCOS are overweight or obese.
• Male-pattern baldness. Hair on the scalp gets thinner and fall out.
• Darkening of the skin. Dark patches of skin can form in body creases like those on the neck, in the groin, and under the breasts.
• Headaches. Hormone changes can trigger headaches in some women.
How PCOS affects your body
Having higher-than-normal androgen levels can affect your fertility and other aspects of your health.
· Infertility
To get pregnant, you have to ovulate. Women who don’t ovulate regularly don’t release as many eggs to be fertilized. PCOS is one of the leading causes of infertility in women.
· Metabolic syndrome
Up to 80 % of women with PCOS are overweight or obese. Both obesity and PCOS increase your risk for high blood sugar, high blood pressure, low HDL (“good”) cholesterol, and high LDL (“bad”) cholesterol.
Together, these factors are called metabolic syndrome, and they increase the risk for heart disease, diabetes, and stroke.
· Sleep apnea
This condition causes repeated pauses in breathing during the night, which interrupt sleep.
Sleep apnea is more common in women who are overweight — especially if they also have PCOS. The risk for sleep apnea is 5 to 10 times higher in obese women with PCOS than in those without PCOS.
· Endometrial cancer
During ovulation, the uterine lining sheds. If you don’t ovulate every month, the lining can build up. A thickened uterine lining can increase your risk for endometrial cancer.
· Depression
Both hormonal changes and symptoms like unwanted hair growth can negatively affect your emotions. Many with PCOS end up experiencing depression and anxiety.
How PCOS is diagnosed
Doctors typically diagnose PCOS in women who have at least two of these three symptoms (17):
• high androgen levels
• irregular menstrual cycles
• cysts in the ovaries
Your doctor should also ask whether you’ve had symptoms like acne, face and body hair growth, and weight gain.
A pelvic exam can look for any problems with your ovaries or other parts of your reproductive tract. During this test, your doctor inserts gloved fingers into your vagina and checks for any growths in your ovaries or uterus.
Blood tests check for higher-than-normal levels of male hormones. You might also have blood tests to check your cholesterol, insulin, and triglyceride levels to evaluate your risk for related conditions like heart disease and diabetes.
An ultrasound uses sound waves to look for abnormal follicles and other problems with your ovaries and uterus.
Pregnancy and PCOS
PCOS interrupts the normal menstrual cycle and makes it harder to get pregnant. Between 70 and 80 % of women with PCOS have fertility problems (18).
This condition can also increase the risk for pregnancy complications.
Women with PCOS are twice as likely as women without the condition to deliver their baby prematurely. They’re also at greater risk for miscarriage, high blood pressure, and gestational diabetes.
However, women with PCOS can get pregnant using fertility treatments that improve ovulation. Losing weight and lowering blood sugar levels can improve your odds of having a healthy pregnancy.
Diet and lifestyle tips to treat PCOS
Treatment for PCOS usually starts with lifestyle changes like weight loss, diet, and exercise.
Losing just 5 to 10 % of your body weight can help regulate your menstrual cycle and improve PCOS symptoms. Weight loss can also improve cholesterol levels, lower insulin, and reduce heart disease and diabetes risks.
Any diet that helps you lose weight can help your condition. However, some diets may have advantages over others.
Studies comparing diets for PCOS have found that low-carbohydrate diets are effective for both weight loss and lowering insulin levels. A low glycemic index (low-GI) diet that gets most carbohydrates from fruits, vegetables, and whole grains helps regulate the menstrual cycle better than a regular weight loss diet.
A few studies have found that 30 minutes of moderate-intensity exercise at least three days a week can help women with PCOS lose weight. Losing weight with exercise also improves ovulation and insulin levels.
Exercise is even more beneficial when combined with a healthy diet. Diet plus exercise helps you lose more weight than either intervention alone, and it lowers your risks for diabetes and heart disease.
There is some evidence that acupuncture can help with improving PCOS, but more research is needed.
Common medical treatments
Birth control pills and other medicines can help regulate the menstrual cycle and treat PCOS symptoms like hair growth and acne.
· Birth control
Taking estrogen and progestin daily can restore a normal hormone balance, regulate ovulation, relieve symptoms like excess hair growth, and protect against endometrial cancer. These hormones come in a pill, patch, or vaginal ring.
· Metformin
Metformin (Glucophage, Fortamet) is a drug used to treat type 2 diabetes. It also treats PCOS by improving insulin levels.
One study found that taking metformin while making changes to diet and exercise improves weight loss, lowers blood sugar, and restores a normal menstrual cycle better than changes to diet and exercise alone.
· Clomiphene
Clomiphene (Clomid) is a fertility drug that can help women with PCOS get pregnant. However, it increases the risk for twins and other multiple births.
· Hair removal medicines
A few treatments can help get rid of unwanted hair or stop it from growing. Eflornithine (Vaniqa) cream is a prescription drug that slows hair growth. Laser hair removal and electrolysis can get rid of unwanted hair on your face and body.
· Surgery
Surgery can be an option to improve fertility if other treatments don’t work. Ovarian drilling is a procedure that makes tiny holes in the ovary with a laser or thin heated needle to restore normal ovulation.
When to see a doctor
See your doctor if:
• You’ve missed periods and you’re not pregnant.
• You have symptoms of PCOS, such as hair growth on your face and body.
• You’ve been trying to get pregnant for more than 12 months but haven’t been successful.
• You have symptoms of diabetes, such as excess thirst or hunger, blurred vision, or unexplained weight loss.
If you have PCOS, plan regular visits with your primary care doctor. You’ll need regular tests to check for diabetes, high blood pressure, and other possible complications.
Main Points
PCOS can disrupt a woman’s menstrual cycles and make it harder to get pregnant. High levels of male hormones also lead to unwanted symptoms like hair growth on the face and body.
Lifestyle interventions are the first treatments doctors recommend for PCOS, and they often work well. Weight loss can treat PCOS symptoms and improve the odds of getting pregnant. Diet and aerobic exercise are two effective ways to lose weight.
Medicines are an option if lifestyle changes don’t work. Birth control pills and metformin can both restore more normal menstrual cycles and relieve PCOS symptoms.
Thyroid
What is Thyroid?
The thyroid is a small gland in your neck that makes thyroid hormones. Sometimes the thyroid makes too much or too little of these hormones. Too much thyroid hormone is called hyperthyroidism and can cause many of your body's functions to speed up. “Hyper” means the thyroid is overactive.
Thyroid
1. When Your Thyroid Goes Awry
3. Symptom: Weight Gain or Loss
1. When Your Thyroid Goes Awry

Does fatigue drag you down day after day? Do you have brain fog, weight gain, chills, or hair loss? Or is the opposite true for you: Are you often revved up, sweaty, or anxious? Your thyroid gland could be to blame. This great regulator of body and mind sometimes goes haywire, particularly in women. Getting the right treatment is critical to feel your best and avoid serious health problems.
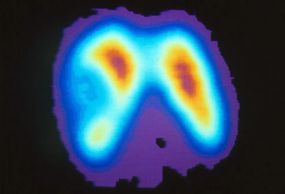
2. What Is the Thyroid Gland?
3. Symptom: Weight Gain or Loss
1. When Your Thyroid Goes Awry

The thyroid is a butterfly-shaped gland in the front of the neck. It produces hormones that control the speed of your metabolism -- the system that helps the body use energy. Thyroid disorders can slow down or rev up metabolism by disrupting the production of thyroid hormones. When hormone levels become too low or too high, you may experience a wide range of symptoms.
3. Symptom: Weight Gain or Loss
3. Symptom: Weight Gain or Loss
3. Symptom: Weight Gain or Loss

An unexplained change in weight is one of the most common signs of a thyroid disorder. Weight gain may signal low levels of thyroid hormones, a condition called hypothyroidism. In contrast, if the thyroid produces more hormones than the body needs, you may lose weight unexpectedly. This is known as hyperthyroidism. Hypothyroidism is far more common.
4. Swelling in the Neck
6. Changes in Energy or Mood
3. Symptom: Weight Gain or Loss

A swelling or enlargement in the neck is a visible clue that something may be wrong with the thyroid. A goiter may occur with either hypothyroidism or hyperthyroidism. Sometimes swelling in the neck can result from thyroid cancer or nodules, lumps that grow inside the thyroid. It can also be due to a cause unrelated to the thyroid.
5. Changes in Heart Rate
6. Changes in Energy or Mood
6. Changes in Energy or Mood

Thyroid hormones affect nearly every organ in the body and can influence how quickly the heart beats. People with hypothyroidism may notice their heart rate is slower than usual. Hyperthyroidism may cause the heart to speed up. It can also trigger increased blood pressure and the sensation of a pounding heart, or other types of heart palpitations.
6. Changes in Energy or Mood
6. Changes in Energy or Mood
6. Changes in Energy or Mood

Thyroid disorders can have a noticeable impact on your energy level and mood. Hypothyroidism tends to make people feel tired, sluggish, and depressed. Hyperthyroidism can cause anxiety, problems sleeping, restlessness, and irritability.
Thyroid
7. Hair Loss
8. Feeling Too Cold or Hot
8. Feeling Too Cold or Hot

Hair loss is another sign that thyroid hormones may be out of balance. Both hypothyroidism and hyperthyroidism can cause hair to fall out. In most cases, the hair will grow back once the thyroid disorder is treated.
8. Feeling Too Cold or Hot
8. Feeling Too Cold or Hot
8. Feeling Too Cold or Hot

Thyroid disorders can disrupt the ability to regulate body temperature. People with hypothyroidism may feel cold more often than usual. Hyperthyroidism tends to have the opposite effect, causing excessive sweating and an aversion to heat.
9. Hypothyroidism
8. Feeling Too Cold or Hot
10. Other Symptoms of Hyperthyroidism

Hypothyroidism can cause many other symptoms, including:
· Dry skin and brittle nails
· Numbness or tingling in the hands
· Constipation
· Abnormal menstrual periods.
10. Other Symptoms of Hyperthyroidism
10. Other Symptoms of Hyperthyroidism
10. Other Symptoms of Hyperthyroidism

Hyperthyroidism can also cause additional symptoms, such as:
· Muscle weakness or trembling hands
· Vision problems
· Diarrhea
Irregular menstrual periods
11. Thyroid Disorder or Menopause?
10. Other Symptoms of Hyperthyroidism
11. Thyroid Disorder or Menopause?

Because thyroid disorders can cause changes in menstrual cycle and mood, the symptoms are sometimes mistaken for menopause. If a thyroid problem is suspected, a simple blood test can determine whether the true culprit is menopause or a thyroid disorder -- or a combination of the two.
12. Who Should Be Tested?
10. Other Symptoms of Hyperthyroidism
11. Thyroid Disorder or Menopause?

If you think you have symptoms of a thyroid problem, ask your doctor if you should be tested. People with symptoms or risk factors may need tests more often. Hypothyroidism more frequently affects women over age 60. Hyperthyroidism is also more common in women. A family history raises your risk of either disorder.
Thyroid
13. Thyroid Neck Check
14. Diagnosing Thyroid Disorders
14. Diagnosing Thyroid Disorders

A careful look in the mirror may help you spot an enlarged thyroid that needs a doctor's attention. Tip your head back, take a drink of water, and as you swallow, examine your neck below the Adam's apple and above the collarbone. Look for bulges or protrusions, then repeat the process a few times. See a doctor promptly if you see a bulge or lump.
14. Diagnosing Thyroid Disorders
14. Diagnosing Thyroid Disorders
14. Diagnosing Thyroid Disorders

If your doctor suspects a thyroid disorder, a blood test can help provide an answer. This test measures the level of thyroid stimulating hormone (TSH), a kind of master hormone that regulates the work of the thyroid gland. If TSH is high, it typically means that your thyroid function is too low (hypothyroid). If TSH is low, then it generally means the thyroid is overactive (hyperthyroid.) Your doctor may also check levels of other thyroid hormones in your blood. In some cases, imaging studies are used and biopsies are taken to evaluate a thyroid abnormality.
15. Hashimoto's Disease
14. Diagnosing Thyroid Disorders
16. Other Causes of Hypothyroidism

The most common cause of hypothyroidism is Hashimoto's disease. This is an autoimmune disorder in which the body attacks the thyroid gland. The result is damage to the thyroid, preventing it from producing enough hormones. Hashimoto's disease tends to run in families.
16. Other Causes of Hypothyroidism
18. Other Causes of Hyperthyroidism
16. Other Causes of Hypothyroidism

In some cases, hypothyroidism results from a problem with the pituitary gland, which is at the base of the brain. This gland produces thyroid-stimulating hormone (TSH), which tells the thyroid to do its job. If your pituitary gland does not produce enough TSH, levels of thyroid hormones will fall. Other causes of hypothyroidism include temporary inflammation of the thyroid or medications that affect thyroid function
17. Graves' Disease
18. Other Causes of Hyperthyroidism
18. Other Causes of Hyperthyroidism

The most common cause of hyperthyroidism is Graves' disease. This is an autoimmune disorder that attacks the thyroid gland and triggers the release of high levels of thyroid hormones. One of the hallmarks of Graves' disease is a visible and uncomfortable swelling behind the ey
18. Other Causes of Hyperthyroidism
18. Other Causes of Hyperthyroidism
18. Other Causes of Hyperthyroidism
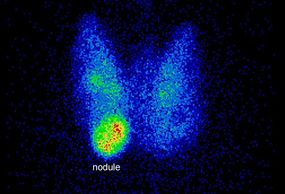
Hyperthyroidism can also result from thyroid nodules. These are lumps that develop inside the thyroid and sometimes begin producing thyroid hormones. Large lumps may create a noticeable goiter. Smaller lumps can be detected with ultrasound. A thyroid uptake and scan can tell if the lump is producing too much thyroid hormone.
Thyroid
19. Thyroid Disorder Complications
19. Thyroid Disorder Complications
19. Thyroid Disorder Complications

When left untreated, hypothyroidism can raise cholesterol levels and make you more likely to have a stroke or heart attack. In severe cases, very low levels of thyroid hormones can trigger a loss of consciousness and life-threatening drop in body temperature. Untreated hyperthyroidism can cause serious heart problems and brittle bones.
20. Treating Hypothyroidism
19. Thyroid Disorder Complications
19. Thyroid Disorder Complications

If you are diagnosed with hypothyroidism, your doctor will most likely prescribe thyroid hormones in the form of a pill. This usually leads to noticeable improvements within a couple of weeks. Long-term treatment can result in more energy, lower cholesterol levels, and gradual weight loss. Most people with hypothyroidism will need to take thyroid hormones for the rest of their lives.
21. Treating Hyperthyroidism
19. Thyroid Disorder Complications
22. Surgery for Thyroid Disorders

The most common option in treating adults is radioactive iodine, which destroys the thyroid gland over the course of 6 to 18 weeks. Once the gland is destroyed, or removed by surgery, most patients must begin taking thyroid hormones in pill form. Another common treatment for hyperthyroidism is antithyroid medication, which aims to lower the amount of hormones produced by the thyroid. The condition may eventually go away, but many people need to remain on medication for the long term. Other drugs may be given to reduce symptoms such as rapid pulse and tremors.
22. Surgery for Thyroid Disorders
22. Surgery for Thyroid Disorders
22. Surgery for Thyroid Disorders

Removing the thyroid gland can cure hyperthyroidism, but the procedure is only recommended if antithyroid drugs don't work, or if there is a large goiter. Surgery may also be recommended for patients with thyroid nodules. Once the thyroid is removed, most patients require daily supplements of thyroid hormones to avoid developing hypothyroidism.
23. What About Thyroid Cancer?
22. Surgery for Thyroid Disorders
23. What About Thyroid Cancer?
Thyroid cancer is uncommon and is among the least deadly. The main symptom is a lump or swelling in the neck, and only about 5% of thyroid nodules turn out to be cancerous. When thyroid cancer is diagnosed, it is most often treated with surgery followed by radioactive iodine therapy or, in some cases, external radiation therapy.
Foods That Help or Hurt Your Thyroid
Salt
Leafy Greens
Leafy Greens

Your thyroid needs iodine to work well. Most people get enough of this element from their diet, usually through fish and dairy products. Make sure you’re using iodized table salt at home. You can tell by looking at the label.
Leafy Greens
Leafy Greens
Leafy Greens

Spinach, lettuce, and other examples are great sources of magnesium, an all-star mineral that plays a huge role in your body processes. Fatigue, muscle cramps, and changes in your heartbeat could be signs that you're not getting enough.
Nuts
Leafy Greens
Seafood

Cashews, almonds, and pumpkin seeds are excellent sources of iron. Brazil nuts help your thyroid in two ways. Not only are they a good source of iron, but they're also rich in selenium, another mineral that supports your thyroid. Just a few each day give you the selenium you need.
Seafood
Seafood
Seafood

Fish, shrimp, and seaweed are great sources of iodine. You need iodine for a healthy thyroid, but avoid large amounts of iodine-rich choices like kelp. That may make your condition worse.
Kale
Seafood
Kale

Could that superstar among superfoods, actually not be quite so awesome? Kale is a mild goitrogen -- in rare cases it prevents the thyroid from getting enough iodine. But kale shouldn't be a problem for you unless you get very little iodine in your diet and you’re eating large amounts of kale. This is also the case for cabbage, broccoli, cauliflower, and Brussels sprouts.
Soy
Seafood
Kale

In rare cases, some of the chemicals found in soy products like soy milk or edamame could hurt your thyroid’s ability to make hormones, but only if you don't get enough iodine and eat large amounts. Just like with kale, if your iodine levels are OK, you probably don’t need to worry about soy.
Site Content
Organ Meats
Thyroid Medication and Your Food
Gluten and Your Thyroid

If you eat things like kidneys, heart, or liver, you might get a lot of lipoic acid. That's a fatty acid in these and some other foods. You can also buy it as a supplement. But if you get too much, it could mess with the way your thyroid works. Lipoic acid could also affect any thyroid medicines you take.
Gluten and Your Thyroid
Thyroid Medication and Your Food
Gluten and Your Thyroid

Gluten is a protein found in wheat, rye, and barley. Unless you've been diagnosed with celiac disease, it probably won’t affect your thyroid. Gluten can damage the small intestines of people with celiac disease. They can have other autoimmune disorders like Hashimoto’s disease (which leads to an underactive thyroid) and Graves' disease (which leads to an overactive thyroid). If you have celiac disease, a gluten-free diet may help prevent these thyroid diseases.
Thyroid Medication and Your Food
Thyroid Medication and Your Food
Thyroid Medication and Your Food

The foods you eat can affect your thyroid medicine. They can slow down how your body absorbs medicine. It can also affect how well it does it.
- Take medicine on an empty stomach, preferably in the morning.
- Some vitamins and antacids can also prevent your medicine from working.
- Ask your doctor or pharmacist for more information about timing your food and other meds around your thyroid treatment.
Thyroid
Exercises for an Under-active Thyroid
If you have an under active thyroid, a condition called hypothyroidism, exercise is probably the last thing on your mind. After all, symptoms like fatigue, swelling, and joint and muscle pain don’t make you want to get up and go.
But experts say that physical activity can help you feel better.
What Type of Workout Should I Do?
If your condition is well controlled, you should be able to do the same physical activity as someone without a thyroid disorder, says John C. Morris, MD, professor of medicine and endocrinology at the Mayo Clinic College of Medicine.
But if you’re just starting an exercise plan or if you’re still dealing with symptoms, low-impact aerobic exercise and strengthening moves are best.
“Low-impact exercise doesn’t apply as much pressure,” says Norma Lopez, MD, an associate professor of endocrinology and metabolism at Loyola University Medical Center. “That’s key, since hypothyroidism can cause pain and swelling in your muscles and joints.”
Try these activities:
Walking: One of the easiest workouts to do. All you need is a pair of comfortable shoes. It gets your heart pumping and burns about 280 calories an hour.
Water aerobics: If you have swelling in your ankles or feet, some exercises may be painful. Water aerobics is a good option. The water holds you up and lowers the impact on your joints.
Yoga: This can stretch and strengthen your muscles. It also helps you focus on breathing. One study found that people with hypothyroidism had better lung strength after practicing yoga breathing for 6 months.
Tai chi: Described as “moving meditation,” this slow-motion form of martial arts is a proven stress-buster. Research shows it can help improve strength, balance, and mood.
Strength training: Whether you lift weights or use your body weight, building muscle helps you burn more calories -- even when you’re sitting still. And that can help you shed extra pounds. Strong muscles also help ease pressure on your joints.
Why Should You Get Moving?
While medication from your doctor is the only way to help your body make more hormones, exercise can help some of the problems that come with hypothyroidism, Morris says.
Working out 3 hours a week for 3 months can put you in better physical and mental health and raise your quality of life.
There are many ways exercise can help:
Boost your mood. “An under active thyroid can cause feelings of depression and anxiety,” Lopez says. Exercise lowers stress and helps your body make more endorphins. This lifts your mood and zaps those sad and anxious feelings.
Help you lose weight. A slow metabolism can cause weight gain and make it hard to shed pounds. Exercise burns calories and builds muscle, which can help you slim down.
Increase your energy. Fighting fatigue or sluggishness? Low-intensity aerobic exercise can help. People who rode an exercise bike for 20 minutes, three times a week, had more energy and less fatigue.
How Can You Get Started?
Before you start any workout routine, see your doctor.
“You need to make sure that your hypothyroidism is under control,” Lopez says. You should have a thyroid that works normally through thyroid-hormone replacement medications before you start.
If you don’t, exercise may make you feel worse. For instance, going for a run could make your already-aching joints hurt even more, Lopez says. Because an under active thyroid often causes shortness of breath, a return to exercise before you’re ready could cause you to wheeze through a workout.
Also, check with your doctor before taking any supplements, like protein powders, to boost your workouts. Some nutrients, like the soy found in shakes, can stop your medications from working like they should, Lopez says.
As with any new exercise routine, start slow. Take breaks if you need them, and stop if it hurts. Once you feel more comfortable, build up to longer, harder workouts.